Unsafe and unethical: bed shortages mean dementia patients with psychiatric symptoms are admitted to medical wards
The Conversation
30 Jun 2025, 02:17 GMT+10

New Zealand's mental health crisis is well documented in the government's 2018 inquiry, He Ara Oranga, which shows one in five people experience mental illness or significant mental distress.
However, an almost singular focus on care of young people obscures the psychiatric needs of older adults.
Failure to account for these needs has resulted in physicians facing pressure to admit psychiatric patients to medical wards that are not designed or resourced to care for them. This compromises patient safety and rights as well as fundamental standards of care.
Our new research highlights the clinical, ethical and legal consequences of this practice and calls for urgent action.
The memory deficits of dementia are well known but the condition also includes psychiatric presentations. These are known collectively as the "behavioural and psychiatric symptoms of dementia" (BPSD). When severe, they can include intrusive behaviour, violence and inappropriate sexual conduct. Such patients require admission and specialist treatment.
However, New Zealand has a severe shortage of psychiatric beds for older adults. Even more concerning is that despite well recognised demographic trends and clinical concerns, bed numbers have decreased over time rather than increased.
Reports that Dunedin plans to slash the number of psycho-geriatric beds by 50% reflect a lack of government insight into the risks this large and growing patient cohort poses.
Hospitals routinely expect medical wards to admit dementia patients presenting with BPSD when no psycho-geriatric bed is available. Yet it is impossible for staff on medical wards to adhere to even basic standards of care.
A lack of single rooms means medical teams cannot provide the security and minimisation of light and noise people with dementia require. Single rooms need to be prioritised for transmissible infections, delirium and terminal care.
Medical wards are also not designed for aggressive patients. People can enter and exit freely, potential weapons (scissors, for example) are accessible, there are no seclusion rooms or low-stimulus areas, and nursing stations are not secure.
Medical staff are not trained in de-escalation or restraint and ward pharmacists are not specialised in the medications required to treat BPSD.
Those presenting with physical or sexual violence also need dedicated security, well beyond what healthcare assistants on "patient watches" can provide. Most healthcare assistants are women, which creates a grossly inadequate level of safety when managing violent male patients.
The experience of Wellington general medicine staff documents numerous assaults on nurses and intrusive and frightening behaviour. Staff have been punched, hit, bitten and threatened. One nurse was stabbed while attending to another patient in a multi-bed room.
Admissions have included physically robust patients who have seriously assaulted family or carers. This includes one man who committed a fatal assault and another who was sexually aggressive and stabbed a family member.
High rates of mixed-gender bedding in hospital wards raise the risk of harm. The United Kingdom banned hospitals from placing men and women in the same room in 2010. Yet despite concerns for patient safety, New Zealand has no prohibition on this practice.
By comparison, Australia proposed a risk stratification approach more than 20 years ago whereby severe dementia patients would be managed in secure units with dedicated security staff and specialist psycho-geriatric care.
This model is used throughout Australia in policy and planning. In New Zealand, severe dementia is defaulted to medical wards even in cases where patients are presenting solely due to extreme violence.
According to the Code of Health and Disability Services Consumers' Rights, patients are entitled to an appropriate standard of care. Admitting someone with dementia to medical wards that cannot meet basic standards of care clearly breaches this right.
BPSD admissions also significantly compromise the rights of other patients. The risks are again demonstrable rather than potential. International media reports have documented male dementia patients assaulting female patients in medical wards without the necessary security measures.
Medical staff in New Zealand hospitals have also witnessed numerous incidents of intrusion and harassment as well as assaults of other patients by dementia patients inappropriately admitted to medical wards with BPSD.
We should also recognise indirect impacts of people with severe dementia being admitted on medical wards. Many patients wait overnight for admission, increasing their risk for complications, and breaching rights to privacy and dignity.
When psychiatric patients occupy medical beds, they contribute to admission delays, complications and rights breaches for medical patients awaiting beds.
Wellington general medicine teams have raised serious concerns about dementia admissions for many years. Yet there are no secure areas and no additional psycho-geriatric beds.
We need to ask why the practice continues when harm is so obvious. The answer appears to be about cost. When physicians relent and admit psychiatric patients, the risks are high but the financial cost is low. The consequences are born by elderly and frail patients seldom able to advocate for themselves.
Change relies on health leaders and funders caring about safety, rights and basic standards of care. Unfortunately, the Wellington experience and the decision to cut beds in Dunedin suggest change will not happen unless physicians consistently refuse the admission of psychiatric patients. But this is a morally distressing position to be put in.
New Zealand must urgently address the shortage of psycho-geriatric beds. Until these are in place, temporary secure accommodation must be made available under the care of mental health specialists.
Medical teams can no longer be expected to manage the mental health crisis as well as their own medical workloads. It is unsafe, unethical and untenable for all involved.
 Share
Share
 Tweet
Tweet
 Share
Share
 Flip
Flip
 Email
Email
Watch latest videos
Subscribe and Follow
Get a daily dose of Auckland Sun news through our daily email, its complimentary and keeps you fully up to date with world and business news as well.
News RELEASES
Publish news of your business, community or sports group, personnel appointments, major event and more by submitting a news release to Auckland Sun.
More InformationInternational
SectionCanadian option offered to Harvard graduates facing US visa issues
TORONTO, Canada: Harvard University and the University of Toronto have created a backup plan to ensure Harvard graduate students continue...
Israel should act fast on new peace deals, Netanyahu says
JERUSALEM, Israel: Israeli Prime Minister Benjamin Netanyahu says that Israel's success in the war with Iran could open the door to...
UN offer rejected in Dreamliner crash investigation
NEW DELHI, India: India has decided not to allow a United Nations (UN) investigator to join the investigation into the recent Air India...
UN climate agency gets 10 percent boost amid global budget cuts
BONN, Germany: Despite widespread belt-tightening across the United Nations, nearly 200 countries agreed this week to increase the...
Mexican President orders review of SpaceX environmental impact
MEXICO CITY, Mexico: Mexican President Claudia Sheinbaum said this week that her government is investigating possible environmental...
Historic ISS mission launches with crew from 4 different nations
CAPE CANAVERAL, Florida: In a landmark flight for three nations and a veteran U.S. spacefarer, a four-member astronaut crew launched...
New Zealand
SectionTerracotta Warriors exhibition to help Australians understand Chinese culture: museum CEO
PERTH, Australia, June 30 (Xinhua) -- The ongoing exhibition of China's world-famous Terracotta Warriors at the Western Australian...
Unsafe and unethical: bed shortages mean dementia patients with psychiatric symptoms are admitted to medical wards
New Zealand's mental health crisis is well documented in the government's 2018 inquiry, He Ara Oranga, which shows one in five people...
Union Minister Mansukh Mandviya participates in 'Sunday on Cycle' program in Gujarat's Bhavnagar
Bhavnagar (Gujarat) [India], June 29 (ANI): Union Minister of Youth Affairs and Sports, Mansukh Mandaviya in the 'Sunday On Cycle'...
Record crowds, global representation highlight 2025 Club World Cup group stage
PHILADELPHIA, June 28 (Xinhua) -- The expanded 2025 FIFA Club World Cup group stage concluded with record-breaking attendance and unprecedented...
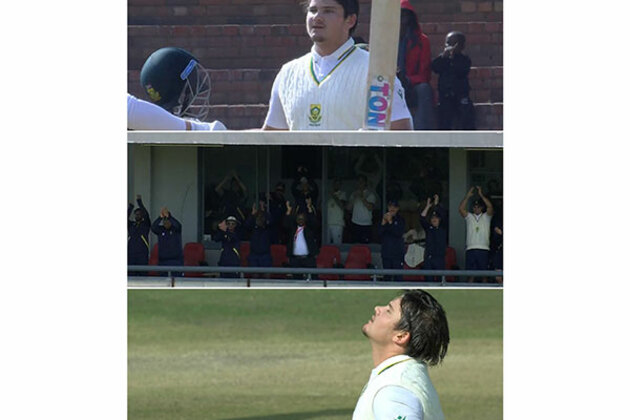
Lhuan-dre Pretorious breaks 61-year-old record to become youngest South African centurion
Bulawayo [Zimbabwe], June 28 (ANI): Young batter Lhuan-dre Pretorious became the youngest South African to score a Test century during...
Lhuan-dre Pretorious breaks 61-year-old record to become youngest South African centurion on debut
Bulawayo [Zimbabwe], June 28 (ANI): Young batter Lhuan-dre Pretorious became the youngest South African to score a Test century during...